ABSTRACT
AIM
To determine rates of hepatitis C (HCV) risk factor ascertainment, testing, and referral in urban primary care practices, with particular attention to the effect of race and ethnicity.
METHODS
Retrospective chart review from four primary care sites in Philadelphia; two academic primary care practices and two community clinics was performed. Demographics, HCV risk factors, and other risk exposure information were collected.
RESULTS
Four thousand four hundred and seven charts were reviewed. Providers documented histories of injection drug use (IDU) and transfusion for less than 20% and 5% of patients, respectively. Only 55% of patients who admitted IDU were tested for HCV. Overall, minorities were more likely to have information regarding a risk factor documented than their white counterparts (79% vs 68%, P < 0.0001). Hispanics were less likely to have a risk factor history documented, compared to blacks and whites (P < 0.0001). Overall, minorities were less likely to be tested for HCV than whites in the presence of a known risk factor (23% vs 35%, P = 0.004). Among patients without documentation of risk factors, blacks and Hispanics were more likely to be tested than whites (20% and 24%, vs 13%, P < 0.005, respectively).
CONCLUSION
(1) Documentation of an HCV risk factor history in urban primary care is uncommon, (2) Racial differences exist with respect to HCV risk factor ascertainment and testing, (3) Minority patients, positive for HCV, are less likely to be referred for subspecialty care and treatment. Overall, minorities are less likely to be tested for HCV than whites in the presence of a known risk factor.
INTRODUCTION
Several studies have suggested that hepatitis C (HBV) manage-ment is suboptimal in primary care settings[1-5]. In fact, only 59% of primary care physicians (PCPs) reported asking patients about HCV risk factors[3]. A similar conclusion was made by another study which found that 46% and 62% of physicians reported that they routinely asked patients about a history of blood transfusion and injection drug use, respectively[4]. Shehab reported that HCV testing is rarely initiated in primary care clinics based on physician identified risk factors such as transfusion prior to 1992 or a history of injection drug use[1]. Similar studies among urban primary care practices, comprising patients at highest risk for exposure to HCV risk factors, have not been reported. Such a study would be important to better assess the feasibility of implementing wide scale risk assessment, testing, and treatment strategies.
The purpose of this retrospective cohort study is to assess the rates of HCV risk factor ascertainment, testing and referral for treatment in urban primary care practices, with particular attention to the effect of race and ethnicity as determined by systematic review of the medical records.
MATERIALS AND METHODS
A retrospective chart review was conducted in four urban primary care clinic sites in Philadelphia. These sites included two federally qualified health clinics serving predominantly minority populations and two university-based primary care practices; a family medicine practice and an internal medicine practice. Each of the four study sites is unique in the population that it serves. Clinic #1 is a community clinic which serves a predominantly Hispanic population (84%), comprised of mostly female patients (66%); in 2005 this clinic served approximately 15 000 patients. Clinic #2 is a community clinic which serves a predominantly black population (65%-70%); this clinic served approximately 7000 patients in 2005. The majority of the patients attending the two community clinics are either uninsured, or covered by a Medicaid HMO. The two university-based practices serve racially diverse populations. Approximately 60% of the patients attending the Family Medicine university-based practice (clinic #3, patient population served in 2005, 23 000) are black. The majority of the patients attending the practice have traditional insurance. Those with Medicare coverage and the uninsured make up a small percentage of the patient population, 6% and 5% respectively. Approximately 45% of the patients attending the Internal Medicine university-based practice (patients served in 2005, 21 000) are black (clinic #4), and the majority of the patients attending the practice have traditional insurance.
Random charts were selected at systematic intervals, based upon practice size, so that a total of approximately 1000 charts were reviewed from each practice. The number of charts required was calculated by taking into account the prevalence of risk factors among minority and non-minority subjects, the rate of risk factors recognized, the proportion of persons at risk screened for HCV and of those who tested positive. All these assumptions were derived from previous studies and from the authors’ experience.
All patient visits in each selected chart were reviewed by a team of trained chart reviewers. No identifying information was collected. Data were available dating back to the patients’ first visit, with a mean of 3.6 years (standard deviation 4.9 years) prior to the patients’ most recent documented visit. Specific data collected included sex, age, race/ethnicity, as well as documentation of HCV risk factors. An HCV risk factor was broadly defined as any potential exposure to HCV; these included injection drug use, blood transfusion prior to 1992, percutaneous exposure as in the case of an exposed health care worker), non-injection drug use, tattoos, body piercing, history of sexually transmitted diseases, incarceration, and unprotected sex[9]. When documentation of an HCV risk factor was identified, it was determined if HCV testing was ordered and if the patient was referred for subspecialty care.
Statistical analysis
Data were collected using a standardized data collection instrument. All chart reviewers were trained and accompanied by an investigator. An investigator (SBT, VJN) re-reviewed at least 10% of all charts at random to check for accuracy. Trained data entry personnel entered the data into data management software (Microsoft Access). All data were analyzed using SAS v 9.14. Descriptive statistics and frequency tables were generated. Chi-square tests and logistic regression were used to assess statistical differences.
RESULTS
Study cohort
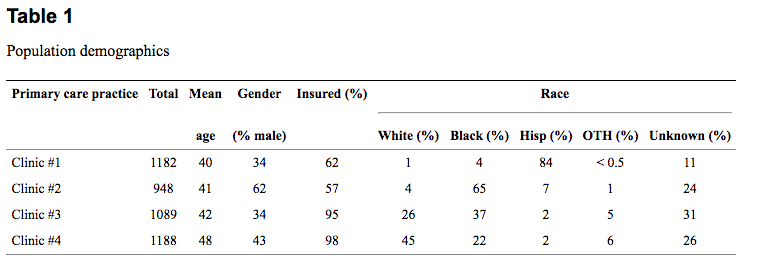
The total number of charts reviewed was 4407. One thousand one hundred eighty two charts were sampled from clinic #1; 948 charts from clinic #2; and 1089 from clinic #3 and 1 188 charts were reviewed from clinic #4 (Table (Table1).1). In order to facilitate a comparison of HCV management practices between races, we included only those charts in which race information was recorded. Approximately 23% of the charts reviewed did not include the race or ethnicity of the patient with clinic #1 having the lowest percentage of undocumented race/ethnicity (11%). Clinic #2 was missing approximately 24% of race/ethnicity documentation as compared to 26% for the Internal Medicine university-based practice and 31% for the Family Medicine university-based practice. Of the 3 413 charts with documented race/ethnicity which were included in the analysis, 1333, 1103, and 846 were reported as black, Hispanic, and white patients, respectively. Racial/ethnic groups were similar with respect to the average age of patients at the time of review (mean age 43). Forty-four percent of blacks were male, as compared to 34% of Hispanics and 45% of whites.
Documentation rate of HCV risk factors and the effect of race/ethnicity
Primary care providers documented a history (positive or negative) of IDU and/ or transfusion, arguably the most important risk factors for HCV acquisition, for 12% and 2% of patients, respectively. Only 0.48% (n = 21) of the total study population (n = 4407) were documented as having a positive history of transfusion prior to 1992. A history of percutaneous exposure as a health care worker was rarely specified (n = 4). Patients’ histories of prostitution, incarceration, tattoos or body piercing were recorded for less than 2% of patients. Ascertainment of a history of non-injection drug use and sexually transmitted diseases occurred for 67% and 34% of patients, respectively.
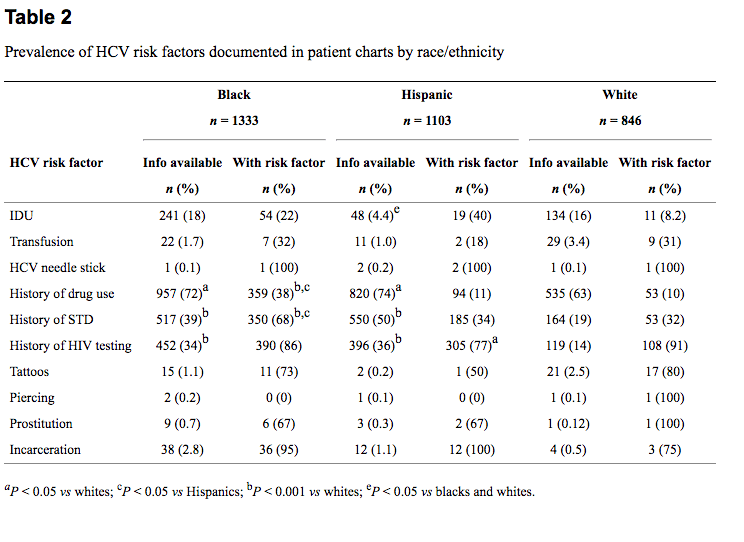
When documentation of HCV risk factor ascertainment was compared between different races/ethnicities, overall, minorities were more likely to have information regarding a risk factor documented than their white counterparts (79% vs 68%, P < 0.0001). Hispanics were much less likely to have had a history of IDU (positive or negative) documented than other groups; (4.4% ascertainment rate compared with 18% and 16% for blacks and whites, respectively) (P < 0.0001). Blacks and Hispanics were more likely to have had a documented history of non-IDU (72% and 74%, respectively) as compared to whites (63%, P < 0.05). Hispanics were more likely to have a chart entry regarding sexually transmitted diseases than were blacks (50% vs 39%) and blacks were more likely to have this history documented than whites (39% vs19%, P < 0.001). Statistical comparisons were not used to assess differences between racial/ethnic groups for prostitution, incarceration, tattoos or body piercing due to the low rate of ascertainment.
Among patients who denied IDU, higher rates of other risk factors were reported among minorities. For example, 64% (29/45) of the minorities who denied IDU admitted non-injection drug use as compared to 31% (5/16) of the whites (P < 0.05). In addition, 25% of minorities (55/216) who denied IDU had a history of an STD documented as compared to 5% (7/123) of whites (P < 0.05).
Overall, females (74%, n = 2 469) were more likely than males (71%, n = 1 818) to have information regarding a risk factor history (positive or negative history) documented in the chart (P = 0.0091). However, among those individuals who had risk factor information documented, males (54%) were more likely to have a positive risk factor history than females (30%) (P < 0.0001). Among individuals with a documented positive HCV risk factor, there was no difference in the percentage of males and females tested for HCV (P = 0.176).
The odds of having documented information regarding HCV risk factors decreased by 1.4% with each additional year of age (P < 0.0001). Among those individuals who had risk factor information documented (n = 3113), the odds of having a positive risk factor history decreased by 1.7% with each additional year of age (P < 0.0001). Among individuals with a documented positive HCV risk factor (n = 1158), the odds of being tested increased by 1.3% with each additional year of age (P = 0.025).
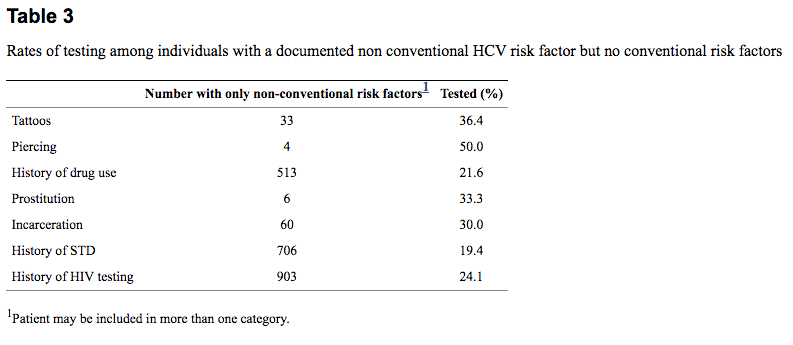
HCV testing
Overall, minorities were less likely to be tested for HCV than whites in the presence of a known risk factor (23% vs 35%, P = 0.004). Of the 12% of patients for whom information regarding IDU was recorded (n = 531), 19% admitted this behavior. Of this group (blacks n = 54, Hispanics n = 19, whites n = 11), 55%-58% were tested for HCV, with no differences among the race or ethnic groups. Of the 21 patients documented as having a history of blood transfusion prior to 1992, approximately 67% were tested for HCV. Because the rate of documentation was so low for a history of transfusion, comparisons between racial/ethnic groups could not be made with respect to the rate of testing in the presence of this risk factor. Thirty-six percent of patients with tattoos and 50% of individuals with body piercing and with no identified other risk factor were tested for HCV (Table (Table3).3). Of those patients with a history of incarceration, 30% were tested. In the absence of IDU or prior blood transfusion, a history of sexually transmitted disease, non-injection drug use, engaging in sexual activity with or as a commercial sex worker, or a history of HIV testing were associated with testing rates of 19%, 22%, 33% and 24%, respectively. Due to the low rate of documentation of risk factors by the physicians, it was not possible to compare rates of testing between racial groups for piercing, incarceration, prostitution, and tattoos.
Among patients who denied risk factors when asked, the proportion tested for HCV was higher for blacks (20%, n = 187) and Hispanics (24%, n = 29) than for whites (13%, n = 123) (P < 0.05).
Overall, seven percent of patients in whom no risk factors were documented (n = 3212) were still tested for HCV. Hispanics (9.9%, n = 848) were more likely to be tested than both blacks (5.4%, n = 737) and whites (6.4%, n = 733) in the absence of any documented risk factor.
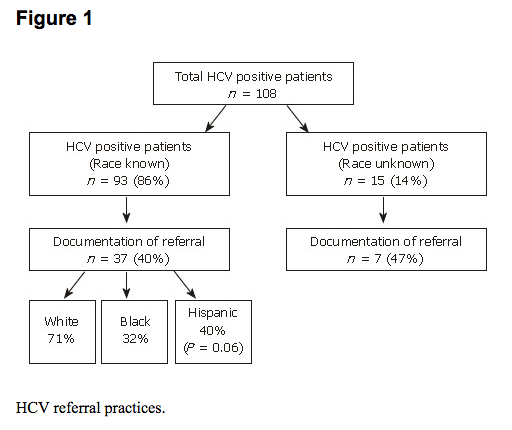
HCV referral practices
Of the 93 patients who were identified as being HCV positive (and for whom race/ethnicity was known), 37 (40%) had chart documentation of referral to a specialist. Of this group, 71% of white patients were referred, as compared to 40% of Hispanics (P = 0.06), and 32% of blacks (Figure (Figure1).1). Among HCV positive patients whose race was not known (n = 15), 47% were referred to a specialist. Of these, 10 patients were from clinic #2, which serves a predominantly black population.
DISCUSSION
Overall, minorities were more likely to have information regarding HCV risk factors documented than their white counterparts. However, the ascertainment of IDU and blood transfusion prior to 1992, arguably the most important risk factors for HCV acquisition, was low, 12% and 1.8% respectively. Perhaps the greatest significance of these findings is that even in populations with expected high rates of risk factors, recommended management practices for risk factor ascertainment are infrequently followed[9].
Overall, minorities were less likely to be tested for HCV than whites in the presence of a known risk factor. The underlying reason for this is unknown but deserves further study. Rates of testing among patients who had a documented history of IDU or blood transfusion prior to 1992 were low, regardless of race. This finding demonstrates that recommendations regarding HCV testing practices are infrequently followed[9–12]. The reason for low rates of testing among minorities in the presence of a risk factor is likely to be multifactorial. Practitioners may be more likely to ask minority patients about risk behaviors, given an implicit understanding of the surrounding urban community and the epidemiology of HCV, but less likely to test if the provider feels that the patient would not be a candidate for treatment or if the patient would not opt for treatment.
Minorities were more likely than non-minorities to be tested for HCV in the absence of a recorded risk factor, or if such a history was denied. This finding could be explained by undocumented factors which might have led to testing, or the more frequent documentation of non-intravenous drug use in this population, which might be, in turn, interpreted as a risk for the acquisition of HCV. Unfortunately, medical record information did not allow us to more carefully assess these factors.
The rate of referral among patients who tested positive for HCV differed among the race groups. Specifically, minorities were less likely than whites to be referred for subspecialty evaluation. Although of potential significance, this finding may have been affected by missing referral information, local resources, as well as patient and provider perception of the need for and benefit of treatment.
Our study is limited in scope due to several factors. We performed the study in a relatively small number of practices which may reflect idiosyncrasies of a few treating physicians or have been affected by patient demographics which were unique to the local area. Moreover, we could not assess whether cultural, educational, or economic factors affected risk assessment and testing practices. Despite these limitations, the low rate of testing in a potentially high-risk population has serious implications; any strategy to test patients at risk for acquisition of HCV must be preceded by a plan that increases the rate of risk factor ascertainment in primary care.
Therefore, recommendations must be developed for physicians to increase the rate of identification of individuals who may have been exposed to HCV in the past as well as appropriate testing. Although primary care physicians are responsible for screening for multiple health problems during a routine health care visit, the benefits of identifying HCV risk factors and infection must not be overlooked. Risk factor screening and identification allows for patients to be educated regarding the risks of injection drug use and needle sharing. Appropriate testing and diagnosis of HCV allows for the patient to be evaluated for treatment and receive counseling regarding alcohol cessation. In addition to physician education, patient education campaigns must also be developed to increase patient compliance with testing recommendations made by their physicians.
ACKNOWLEDGMENTS
The authors thank Sidney Cohen, MD for his assistance in preparation of the manuscript.
COMMENTS
Background
The increasing prevalence of hepatitis C virus (HCV) infection in the United States makes it an important challenge for primary care physicians (PCPs) and subspecialists. There are several potential benefits to diagnosing hepatitis C in a primary care setting.Diagnosis provides the patient with the opportunity to be counseled regarding behaviors that may transmit the infection to others such as sharing needles in the context of IDU. Diagnosis also allows the health care provider to educate the patient regarding behaviors that may hasten the progression of liver disease such as alcohol intake. Furthermore, early diagnosis allows the patient to be provided with appropriate preventive services such as hepatitis A and B vaccines. Lastly, early diagnosis allows the patient to be evaluated for hepatitis C therapy at a time when treatment may be more effective; prior to progression to fibrotic liver disease.
Research frontiers
Several studies have suggested that hepatitis C management is suboptimal in primary care settings. The purpose of this retrospective cohort study is to assess the rates of HCV risk factor ascertainment, testing and referral for treatment in urban primary care practices, with particular attention to the effect of race and ethnicity as determined by systematic review of the medical records.
Related publications
This publication is the first to result from our studies related to HCV management in primary care settings. Three additional manuscripts are in preparation. However, there are several articles, cited throughout this manuscript, from other investigators, that can provide additional information related to HCV management in primary care.
Innovations and breakthroughs
Very few studies have examined hepatitis C risk assessment, testing and referral for treatment in urban primary care settings. Moreover, no studies have examined racial differences within these practices. The findings indicate that (1) Documentation of an HCV risk factor history in urban primary care is uncommon, (2) Racial differences exist with respect to HCV risk factor ascertainment and testing, and (3) Minority patients, positive for HCV, were less likely to be referred for subspecialty care and treatment. Overall, minorities were less likely to be tested for HCV than whites in the presence of a known risk factor.
Applications
The findings presented may be applied in a number of settings where advances in the identification, testing and referral of primary care patients, specifically racial and ethnic minorities are sought. The results of this study may be of interest to epidemiologists and other public health professionals. The findings of this study address a deficit in the literature related to HCV in minorities and provide the background for future studies and intervention endeavors aimed at improving HCV identification and management in primary care settings.
Peer review
The results show that risk factors are often missed and minority patients are less likely to be tested for HCV and to be referred for treatment. The authors conclude that, although their investigation has some selection biases, the results indicate the existence of a consistent reservoir of infection in subgroups of patients, [specifically] black and Hispanic. Although “expected” given the characteristics of the population selected, the results are interesting.
REFERENCES
Click here to read the original article.

